What is Irritable Bowel Syndrome?
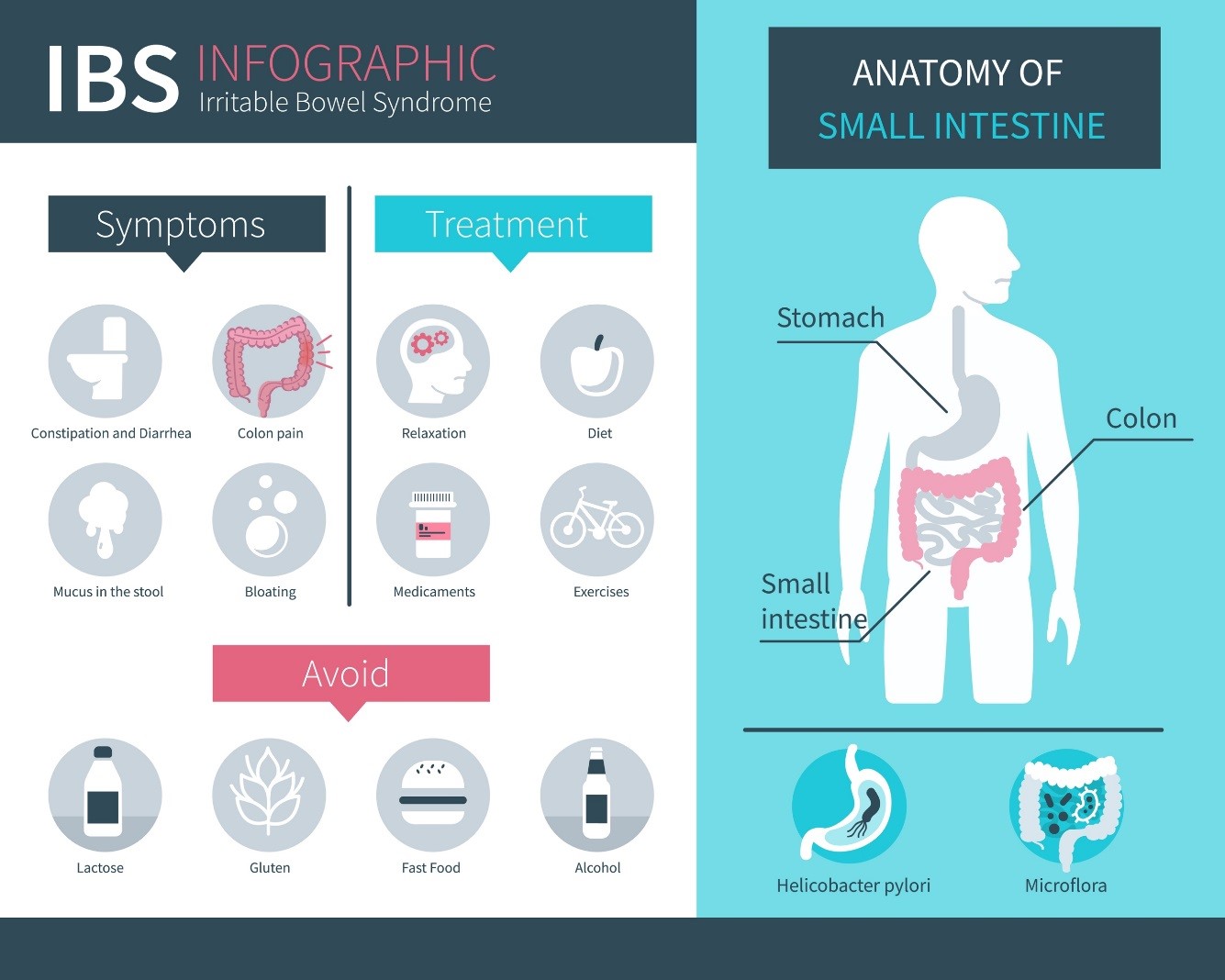
Irritable Bowel Syndrome (or IBS) is a chronic disorder of bowel function. IBS can lead to alternating episodes of constipation or diarrhea. It can cause abdominal pain and bloating that comes and goes with time. There are different types of IBS including IBS with constipation, IBS with diarrhea, or IBS with mixed symptoms (which means you may have both constipation and diarrhea).
IBS is quite common. About 10-15% of people in North America suffer from IBS. However, only about 5-7% of adults have officially been diagnosed with IBS by their doctor. It is almost twice as common in women as in men.
Causes

Courtesy of @infectedluna via Unsplash
The cause(s) of IBS remains unclear. There may be some factors that affect nerves and muscles that control the sensation and movement of the intestines. These factors include:
- inflammation (or swelling)
- changes in gut bacteria
- food sensitivities
- family history
Most of these reasons are still being investigated. Tell your doctor about your symptoms. Seek more immediate medical attention if you have:
- persistent or severe pain in your belly
- vomiting
- fever
- blood in your stool
- failure to pass gas
- lower back pain
- unintended weight loss
It is also important to tell your doctor if anyone in your family has had colon or rectal cancer.
Diagnosis
Your doctor will decide which tests (if any) will help evaluate your symptoms. Your symptoms, as well as a physical and rectal exam, are often all that are needed to diagnose IBS. Your doctor may order some of the following tests:
Fecal occult blood test: This test checks the stool for signs of blood that cannot be seen with the naked eye.
Lab tests: Your doctor may check for blood count, hormones, glucose, kidney function, etc. You may even be tested for celiac disease if you mostly have diarrhea.
Sigmoidoscopy or colonoscopy: These tests use a flexible tube to look at your small and large intestines.
Abdominal x-ray: This test can show an obstruction or stool in the intestines.
Computed tomography (CT scan) or magnetic resonance imaging (MRI): These studies can take pictures of your organs and your bowels so your doctor can see if there are any masses or abnormal findings.
Treatment
Initially IBS can be treated with lifestyle and diet modifications. If these don’t help, there are over-the-counter and prescription medications that your doctor may recommend.
 Lifestyle and Diet
Lifestyle and Diet
- Limit gas-producing foods (also called high-FODMAP). These include:
- fructose (sugar found in fruit)
- lactose (sugar in dairy)
- fructans (in wheat, onions, garlic)
- galactans (in beans, lentils, soybeans)
- polyols (sugar alcohols & fruits that have pits or seeds such as avocado, apples, peaches, plums)
- Avoid foods that make your symptoms worse
- Avoid carbonated drinks (especially sodas with high-fructose corn syrup)
- Add more soluble fiber to your diet. Soluble fiber can benefit those with constipation but introduce it into your diet slowly to avoid cramping and bloating.
Medications
There have been many studies done to find the best treatment for IBS. However, only a few therapies have been shown to improve the symptoms of IBS. These include:
- Some antispasmodic medications (such as dicyclomine)
- Peppermint oil
- Anti-diarrheal medications (such as loperamide)
- Osmotic laxatives (such as polyethylene glycol)
- Medications like linactolide or lubiprostone may help with constipation
- Probiotics are good bacteria. These have shown promise in helping reduce IBS symptoms
- Some antidepressant medications (such as selective serotonin reuptake inhibitors or tricyclic antidepressants) can provide symptom relief and reduce pain
- Alosteron (5HT3 antagonist) is a medication that can help severe IBS with diarrhea. However there are strict regulations for its use due to severe side effects.
As with any medication, it is important to consult your doctor before beginning treatment.
Take Home Points
- IBS is quite common and may include symptoms such as:
- diarrhea
- constipation
- abdominal pain
- bloating
- a combination of these
- Many causes and treatments of IBS are still being investigated.
- Diet change is a good first step to help improve your symptoms.
- Much fewer people have been diagnosed with IBS than those who actually have this condition, therefore it is important to talk to your doctor about your symptoms to determine the most appropriate way to diagnose and treat IBS.
Resources
- American College of Gastroenterology IBS Factsheet: http://patients.gi.org/topics/irritable-bowel-syndrome/
- National Institutes of Health IBS Factsheet: https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome
References
- Bharucha AE, Dorn SD, Lembo A, Pressman A. American Gastroenterological Association medical position statement on constipation. 2013;144(1):211–217.
- Brandt LJ, Bjorkman D, Fennerty MB et al. Systematic review on the management of irritable bowel syndrome in North America. Am J Gastroenterol 2002;97 (11 Suppl): S7–S26.
- Brandt LJ, Prather CM, Quigley EM et al. Systematic review on the management of chronic constipation in North America. Am J Gastroenterol 2005;100 (Suppl 1): S5–S21.
- El-Salhy M, Gundersen D, Gilja OH, Hatlebakk JG, Hausken T. Is irritable bowel syndrome an organic disorder? World J Gastroenterol 2014; 20:384–400.
- Ford AC, Moayyedi P, Lacy B, Lembo A, Saito Y, Schiller L, Soffer E, Spiegel B, Quigley EM et al. American College of Gastroenterology Monograph on the Management of Irritable Bowel Syndrome and Chronic Idiopathic Constipation. Am J Gastroenterol 2014;109:S2-S26.
- Longstreth GF, Thompson WG, Chey WD et al. Functional bowel disorders. Gastroenterology 2006;130:1480–1491.
- Muller-Lissner SA, Kamm MA, Scarpignato C, Wald A. Myths and misconceptions about chronic constipation. Am J Gastroenterol 2005; 100:232–242.
- Rao SS, Ozturk R, Laine L et al. Clinical utility of diagnostic tests for constipation in adults: a systematic review. Am J Gastroenterol 2005;100(7):1605
- Sikirov D. Comparison of straining during defecation in three positions: results and implications for human health. Dig Dis Sci 2003; 48:1201–1205.
- Talley NJ, Zinsmeister AR, Van Dyke C, Melton LJ et al. Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroentergology 1991;101(4):927.
- 2008 Physical Activity Guidelines for Americans. Office of Disease Prevention and Health Promotion.
Author Information

Isabel Prieto
Isabel Prieto is currently a fellow at the University of South Florida in the Division of Female Pelvic Medicine & Reconstructive Surgery. She completed her medical school training at Ponce Health Sciences University in Ponce, Puerto Rico and went on to complete her residency training in Obstetrics & Gynecology at the University of South Florida.
No conflicts of interest to report.

Allison Wyman
Allison Wyman, MD, FACOG is an Assistant Professor of Female Pelvic Medicine Reconstructive Surgery, Department of Obstetrics and Gynecology at Morsani College of Medicine, University of South Florida located in Tampa, Florida. She completed her residency in Obstetrics and Gynecology at University Hospitals Case Medical Center/Case Western Reserve University School of Medicine, followed by a three-year fellowship in Female Pelvic Medicine and Reconstructive Surgery at the University of South Florida.
No conflicts of interest to report.