Noelle DeSantis, MS, RDN, CDN
Download: Nutrition for Mental Health_FFHA2020
Nutrition plays a key role in promoting mental health. A diet that provides all essential nutrients will prevent any deficiencies, which may  contribute to mental health conditions. Proper nutrition, including adequate fiber intake, promotes healthy gastrointestinal (GI) function. Food choices can impact our mood and even future food choices. Nutrition can impact mental health conditions such as, but not limited to:
contribute to mental health conditions. Proper nutrition, including adequate fiber intake, promotes healthy gastrointestinal (GI) function. Food choices can impact our mood and even future food choices. Nutrition can impact mental health conditions such as, but not limited to:
- Depression
- Anxiety disorder
- Schizophrenia
- Obsessive-compulsive disorder
Unfortunately, nutrition is often overlooked when treating mental health conditions. Without proper guidance and support from a qualified healthcare professional, it may be difficult to make diet changes and stick with them. With mental health disorders impacting an estimated 264 million people globally, and depression one of the main causes of disability worldwide, it is an important topic.
Where Food Meets Mental Health
Our food choices, mood and mental health are very interwoven. Our current mood drives food choices. Our food choices can drive our mood and future choices. This impacts not only our mental health; it can lead to other chronic diseases too. When the food choices are consistently snack foods with few nutrients, we increase the risk of nutrition-related diseases such as type-two diabetes and hypertension. Some mental health conditions can cause changes in appetite. Skipping meals can lead to deficiencies of important nutrients, making matters worse. Cravings are also associated with mental health conditions. Carbohydrate cravings are correlated with low serotonin levels. Promoting healthy levels of serotonin can be accomplished by a healthy, balanced diet, which would decrease cravings.
Our food choices also impact the health of our gastrointestinal (GI) tract, also known as the gut. What we eat can affect the types and the number of bacteria in our gut. The bacteria is very important for our health. While we all have some pathogenic, or “bad” bacteria in our gut, we also have symbiotic or “good” bacteria as well. The good bacteria help protect us from bad bacteria. They also support healthy immune function and healthy GI function overall.
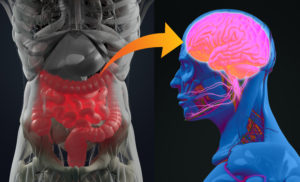 You may be wondering what your gut has to do with mental health, and the answer is quite a bit! When we eat foods that are rich in fiber, the fibers are not digested and absorbed by us. They make their way to the large intestine where bacteria get to ferment them. Fiber can be thought of as the preferred source of food for the bacteria in the gut. Feeding good bacteria helps them grow. In turn, this increases the products the bacteria make which benefit us. These products include nutrients such as short chain fatty acids, vitamin K, biotin, and neurotransmitters.
You may be wondering what your gut has to do with mental health, and the answer is quite a bit! When we eat foods that are rich in fiber, the fibers are not digested and absorbed by us. They make their way to the large intestine where bacteria get to ferment them. Fiber can be thought of as the preferred source of food for the bacteria in the gut. Feeding good bacteria helps them grow. In turn, this increases the products the bacteria make which benefit us. These products include nutrients such as short chain fatty acids, vitamin K, biotin, and neurotransmitters.
The short chain fatty acids are the primary source of fuel for the cells in our GI tract. They help us effectively digest and absorb the nutrients we need to feel well. The bacteria can also produce a variety of neurotransmitters. These are messengers that allow communication between our neurons. One of the neurotransmitters produced is serotonin.
If you have not heard of serotonin, many people refer to it as the “mood” neurotransmitter. It is estimated that 90% of our serotonin is produced in the gut. In addition to regulating mood, serotonin is involved in regulating sleep, appetite and other body functions. These all can impact mental health. For example, our body needs enough serotonin to produce melatonin, the hormone that promotes sleep. Sleep is an important part of managing mental health. Low serotonin leads to increased carbohydrate cravings, can interfere with sleep quality, and can make depression worse. There are a number of nutrients required to produce serotonin. If your body isn’t getting the right nutrients, you may start craving certain foods. Eating sugary foods and refined carbohydrate foods will satisfy cravings short term. But they will lead to a spike and a drop in blood sugar which leads to more cravings. This cycle can negatively affect your mental health.
Helpful Diet Patterns
Some diet patterns have been found to reduce risk of mental disorders, depression, and cognitive health disorders. One of these is a Mediterranean-style diet pattern. The Mediterranean diet is associated with a 30% reduced risk of depression. This diet pattern has benefits for both adults and adolescents. The pattern is rich in:
- Fruits
- Vegetables
- Whole grains
- Fish
- Lean proteins
- Nuts and seeds
When compared with the western diet that is comprised of more processed foods and added sugar, it is richer in fiber, nutrient dense foods and healthy fats. These nutrients are what are thought to be protective against mental health conditions.
Small changes are easier to maintain than trying to overhaul your whole diet pattern. Starting with a goal such as decreasing added sugar and processed foods is a great place to start when promoting mental health.
Key Nutrients
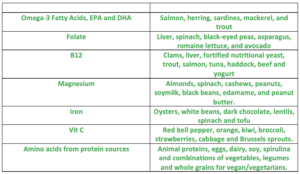
Studies show that people with mental health conditions are often lacking in certain dietary nutrients, essential vitamins, minerals, and omega-3 fatty acids. The most common nutritional deficiencies seen in people with mental health conditions are Omega-3 fatty acids, B vitamins, minerals and amino acids.
Nutrient deficiencies can arise for various reasons. These include:
- Picky eating habits
- Lack of variety in the diet
- Poor absorption due to medications or bacterial overgrowth
- Avoidance of food groups due to allergies, intolerance or preference
- Physical limitations
- Poor appetite
- Food insecurity
It is important to make sure you meet your nutrient needs for all vitamins and minerals. The chart below can help you add variety to your diet and make sure you are getting mood-boosting nutrients you need daily.
Other Considerations
Genetics
There are genes that may be associated with mental health issues. It is important to remember that just because you have a specific gene it does not mean that it is your destiny. Our lifestyle and environment also influence our gene expression. This is something that will vary person to person, and is another topic of its own. An example of how genes can affect nutrition and mental health is the connection between the MTHFR gene and depression. People with this gene may have reduced MTHFR enzyme activity, which can affect the level of the nutrient Folate in the body. This can increase the risk of depression.
Medications
Many people managing mental health disorders will be prescribed medications. It is very important to consider the side effects of these medications. It’s also important to note any food/drug interactions. Certain medications may increase or decrease appetite. A decreased appetite will impact your overall intake of essential nutrients. On the other hand, increased appetite can lead to excess calorie intake and can lead to weight gain. Additional body weight can make physical activity more difficult and impact mental health further.
Take Home Points
- A healthy balanced diet pattern with nutrient dense foods can help prevent and manage mental health disorders.
- Healthy choices for mental health include:
- Avoid added sugar, highly processed foods, and sugary beverages.
- Eat adequate fiber daily to promote a healthy gut microbiome.
- Eat adequate protein to provide building blocks for neurotransmitters.
- A balanced diet includes vegetables, fruits, whole grains, legumes, nuts, seeds, fish and other lean protein and healthy unsaturated fat.
- Make sure to get plenty of restful sleep and regular physical activity.
References
Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: an endocrine organ. Arch Med Sci. 2013;9(2):191–200. doi:10.5114/aoms.2013.33181
Gelinda Deacon, Christine Kettle, David Hayes, Christina Dennis & Joseph Tucci (2017) Omega 3 polyunsaturated fatty acids and the treatment of depression, Critical Reviews in Food Science and Nutrition, 57:1, 212-223, DOI: 10.1080/10408398.2013.876959
Jacka, F.N., O’Neil, A., Opie, R. et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med 15, 23 (2017). https://doi.org/10.1186/s12916-017-0791-y
Lakhan, S.E., Vieira, K.F. Nutritional therapies for mental disorders. Nutr J 7, 2 (2008). https://doi.org/10.1186/1475-2891-7-2
O’Neil A, Quirk SE, Housden S, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. 2014;104(10):e31–e42. doi:10.2105/AJPH.2014.302110
Owen, L., & Corfe, B. (2017). The role of diet and nutrition on mental health and wellbeing. Proceedings of the Nutrition Society, 76(4), 425-426. doi:10.1017/S0029665117001057
Psaltopoulou, T., Sergentanis, T.N., Panagiotakos, D.B., Sergentanis, I.N., Kosti, R. and Scarmeas, N. (2013), Mediterranean diet, stroke, cognitive impairment, and depression: A meta‐analysis. Ann Neurol., 74: 580-591. doi:10.1002/ana.23944
Strandwitz P. Neurotransmitter modulation by the gut microbiota. Brain Res. 2018;1693(Pt B):128–133. doi:10.1016/j.brainres.2018.03.015
Author Information

Noelle DeSantis, MS, RDN, CDN is a registered dietitian nutritionist, specializing in integrative and functional nutrition. Noelle received her Bachelor of Science in Nutrition from San Diego State University, and her Master’s Degree in Nutrition from University at Buffalo. She works for Buffalo Nutrition and Dietetics, PLLC, specializing in neurological disorders out of their office at DENT Neurologic Institute in Buffalo, NY. www.buffalo-nutrition-and-dietetics.com
No conflicts of interest to report.