Lisa Hickman, M.D.
Download: Understanding the Impact of a Vaginal Delivery on the Pelvic Floor_FFHA2020
 Having a baby can be one of the most exciting and scary times in a person’s life. There is a lot of anticipation about what the new baby will be like, how an expectant parent’s life will change, and both how and when the delivery will occur. In the United States, most people will go into labor on their own and have a vaginal birth. In this article you will learn about:
Having a baby can be one of the most exciting and scary times in a person’s life. There is a lot of anticipation about what the new baby will be like, how an expectant parent’s life will change, and both how and when the delivery will occur. In the United States, most people will go into labor on their own and have a vaginal birth. In this article you will learn about:
- The changes that occur during a normal vaginal delivery
- How these changes impact the pelvic floor muscles and vagina
- How to promote healthy healing after delivery
What anatomic changes occur during labor and a normal delivery?
Many changes occur before and during labor to prepare for delivering a baby. Late in the pregnancy, your cervix will likely begin to thin and dilate. The baby’s head may move deeper in your pelvis. This can cause a pressure sensation, frequent urination and, for some, urinary leakage. Your obstetric provider may check your cervix in the later portion of your pregnancy. This exam is to assess the cervix and baby’s location.
Once you are in labor, the cervix continues to dilate and thin. At the same time, the baby’s head moves deeper into the pelvis. During this process your bag of water (the amniotic sac) may spontaneously break, if it has not done so already. This causes you to leak out the fluid around the baby. Alternatively, your provider may break your water with a small hook during an exam. This is not painful.
During labor, your obstetric team may periodically evaluate your progress by checking your cervix. Once the cervix is paper thin, completely dilated (about 10cm), and the baby’s head is low in the pelvis, you will be able to begin pushing.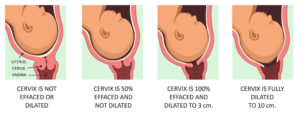
During labor, the vagina and surrounding muscles must stretch significantly to deliver a baby. Before delivery, these and other muscles in the body have already started to relax due to hormone changes in pregnancy. This relaxation may cause heartburn (acid reflux) and/or urine leakage. The pelvic floor muscles are a bowl-shaped group of muscles that support the uterus, vagina, bladder and rectum. Late in pregnancy, these muscles begin to relax, too. This is important as these muscles gradually stretch in labor, up to 200%, for delivery of a baby.
Most first time birthing parents will have at least a little tear in the vagina and/or perineum (space between the vagina and anal opening) from the baby coming through the birth canal. These tears may require stitches, depending on the location and severity. Minor tears often do not need stitches. More severe tears may extend down toward or through the anus and/or rectum and require many stitches. Some people may also have injury to the pelvic floor muscles even if there was no tear. This is believed to happen from the stretching and pressure in the pelvic structures (nerves, muscles and the non-muscular support tissue) during delivery. Birth-related pelvic floor injuries are thought to contribute to some future problems, including bowel and bladder control issues and relaxation of the pelvic organs, also known as prolapse.
There are no specific things you can do to completely prevent vaginal tears during delivery. Some techniques are thought to reduce the risk of having a more severe tear. Warm compresses applied to the perineum during labor and your obstetric provider supporting the perineum during delivery may help.
How should you care for your bottom after a vaginal delivery with or without a birth laceration?
Regardless of whether or not an individual has a tear in or around the vagina, there are things that can be done during recovery to promote healthy healing.
These include:
- Perineal care: Keep your bottom clean and dry. Change your pad frequently. Cleanse with unscented soaps. Use a squirt bottle with warm water (a ‘peri-bottle’) to rinse off after using the toilet. Pat your bottom dry with a clean towel or use a hair dryer on the cool setting. Wash your hands frequently, especially before and after touching your incision.
- Ice packs: Similar to sports injuries, ice can be a useful tool to reduce pain and swelling. Ice should be applied for no longer than 20 minutes at a time. Do not apply directly to the skin.
- Pain medications, both topical and oral: Over the counter medications, such as ibuprofen and acetaminophen, should be the first line treatments for perineal pain and discomfort. Non-steroidal medications, such as ibuprofen, are also helpful to reduce inflammation and swelling. There are numbing medications that your obstetric provider can recommend to apply directly to the painful area. These are available in the form of gels, ointments and sprays. These medications act to temporarily reduce discomfort in the area they are applied.
- Sitz baths: Soaking your bottom for 10 minutes at a time, two to three times a day, can be very helpful to promote healing. You can choose the temperature of the water that is most comfortable. Epsom salts can be added if desired, but are not necessary. Some hospitals provide sitz baths that can be used with your toilet. You can also fill your bathtub, if you have one, with a couple inches of water. After a sitz bath, pat dry your bottom with a clean towel or use a hair dryer on a cool setting.
- Witch hazel pads: These can have a cooling effect and provide relief. They can also be used to help with hemorrhoid discomfort.
- Stool softeners: Keeping your stools soft but formed during the healing process is important. This prevents you from having to strain with bowel movements. Many individuals worry about pain associated with the first bowel movement after having a baby. Drinking lots of water (two to three liters a day) and taking stool softeners can help with this. Some common stool softeners include docusate, milk of magnesia, and polyethylene glycol. These can be purchased at your local pharmacy. Use the medications as directed on the packaging. To achieve the desired stool consistency, you may need to take more than one medication. This should be used during the initial healing period. People with more extensive tears should continue these medications for at least the first six weeks after delivery.
- Pelvic muscle exercises (Kegels): It is not uncommon for individuals to have decreased pelvic muscle strength in the initial postpartum period. Performing pelvic muscle squeezes, also known as Kegel exercises, can be a convenient way to strengthen these muscles. Like any sports injury, however, resting these muscles during the initial period is important. Kegel exercises should not be performed until several weeks after delivery, when pain has resolved, and there has been enough time for healing to occur. Once starting Kegels, you should strive to perform sets of 10 at least 3 to 4 times a day to have an impact on muscle strength.
What is the recovery after a normal vaginal delivery?
Many individuals will feel some soreness and discomfort after a vaginal delivery. This is common especially during the first few weeks. This pain should be managed with the previously described over-the-counter pain medicines and other strategies. If your pain is not controlled, you should contact your obstetric provider. Some people may also experience swelling of the vulva and vagina. Ice packs and non-steroidal anti-inflammatory medications can help with this.
Vaginal bleeding, called lochia, is common after a vaginal delivery. It is generally heaviest during the first week after delivery and should decrease thereafter. The majority of individuals have lochia during the first 4 weeks postpartum. A small number of people may have some spotting up to 6 weeks. If you are still spotting at 6 weeks, you should mention it to your obstetric provider at your follow-up visit. Also, if at any time the discharge looks like pus or is foul smelling, you may have an infection. This would also be a sign to call your obstetric provider.
What is pelvic floor physical therapy?
Pelvic floor physical therapy is a specialized type of physical therapy in which a specialist evaluates your core and pelvic floor muscles. As part of this assessment, they may evaluate your ability to contract different muscles in these areas, and assess your strength and endurance. Based upon this, the physical therapist will develop a plan aimed at improving your strength and function. Helping individuals to properly perform Kegel exercises is one aim. There are also many other tools and techniques the therapist can use. For certain people, such as those with advanced tears, bowel control problems, and/or urine leakage, a pelvic floor physical therapy referral may be very helpful to promote recovery. For individuals with lesser tears, an obstetric provider may be able to teach about the proper way to do a Kegel exercise.
Does a cesarean section prevent pelvic floor problems?
No, a C-section does not completely reduce the risk of future pelvic floor problems. There is increased pressure and stretching of the pelvic floor muscles throughout the later portion of a pregnancy. This happens as the baby grows larger and moves deeper into the pelvis. This pressure may contribute to urine leakage in the pregnancy. For some individuals, urine leakage may also continue for a period of time after delivery. A C-section does avoid the direct impact of a vaginal delivery on the pelvic floor, thereby preventing muscle, nerve and support tissue injury. There is still the general effect of pregnancy, however, which contributes a lesser degree to future pelvic floor problems.
Take Home Points
- During a normal vaginal delivery, there is significant stretching of the pelvic floor. This can result in some pelvic or vaginal injury that may or may not require a repair.
- There are many steps an individual can take after delivery to promote healthy healing.
- C-sections do not completely prevent future pelvic floor problems.
Author Information

Lisa Hickman, M.D. graduated from the Ohio State University College of Medicine. She completed her residency in Obstetrics and Gynecology at the Cleveland Clinic and is currently a fellow in Urogynecology and Reconstructive Pelvic Surgery at the Cleveland Clinic. She has a special interest in the impact of childbirth on the pelvic floor.
No conflicts of interest to report.