Sarah Bradley, MD
Vaginitis_FFHA2019_English
Vaginitis is inflammation of the vagina. There are many causes of vaginitis, infectious and non-infectious. About a third of women will experience some type of vaginitis in their lifetime. Vaginitis can occur at any point during a woman’s life but is most common after puberty and before menopause.
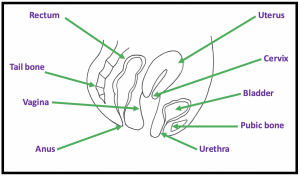
The Normal Vagina
The vagina is a tube that connects the womb (uterus) to the outside world. It lies between the bladder and the rectum. The end of the vagina is connected to the uterus (womb) by the cervix. In women who have undergone hysterectomy, their uterus has been removed and most but not all have had their cervix removed as well. Once the uterus is removed, a woman will no longer have menstrual bleeding (periods). Women with or without a uterus may still develop vaginitis.
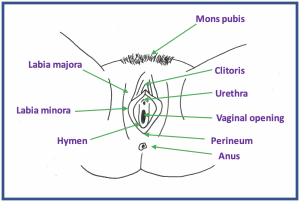
 The Normal Vulva
The Normal Vulva
The vulva is the skin and surrounding structures just outside of the vagina, also called the external genitalia. The hymen is a partial thin membrane near the entrance to the vagina. The external genitalia include the skin folds of the labia (lips), both the labia majora (outer lips) and the labia minora (inner lips). The clitoris is a sensitive female sex organ that lies above the urethra. The skin between the vagina and anus is called the perineum. The skin and the underlying fat pad near the pubic bone is the mons pubis.
What Does a Normal Vulva Look Like?
You can look at the skin surrounding the outside of the vagina by using a hand mirror. Knowing what your skin looks like around the vulva, especially when you do not have any symptoms, is a good idea. The normal look of external genitalia in women varies a great deal. Labia minora range in size and may be up to 2 inches wide. Sometimes the lips are uneven. This is normal. Knowing what the normal color of your skin is and watching for any changes in color such as whiteness, dark spots, redness, cracks in the skin, sores or bumps is helpful. You should tell your doctor if you have any of these changes.
How Can I Best Care for My Vagina and Vulva?
The moist surfaces of the vagina and outer skin are delicate. Washing with harsh soaps, washing too frequently, or rubbing while washing or drying can irritate the skin. Washing with plain, warm water and using your hands to splash water is best. If you desire to use soap, ask your gynecologist or nurse practitioner what may be safest. It is not necessary to wash the vulva every day. Do not use wipes (even baby wipes), deodorants, douches, or other cosmetic products on this skin. Be cautious of these products even if they are meant to be used on the vulva or vagina. This does not mean they cannot cause problems. Gently pat skin dry after washing. Avoid rubbing with a towel or using a hair dryer. Avoid tight-fitting clothing and undergarments in this area. When washing your clothes use a mild or hypo-allergenic detergent. If you need to use pads for menstrual periods or for leakage of urine, the best ones are cotton or hypoallergenic products. Changing them regularly is helpful. Removing the pubic hair from the external genitalia by any means is not recommended. There is no medical reason to remove pubic hair. All methods can increase your risk of infection or skin damage.
What Is Normal Vaginal Discharge?
It is normal to have vaginal discharge. This is usually clear or white and without a strong odor. The consistency and color of your discharge may change during your menstrual cycle, pregnancy, or after menopause. Vaginal discharge is made mostly of water and the normal bacteria of the vagina. Sometimes the amount of discharge is more than a person would like, especially on certain birth controls or during pregnancy, but this does not mean there is a medical problem. Normal discharge, while it may vary in amount, does not cause itching or pain. It just feels wet. Vaginal discharge helps keep the walls of the vagina moist, and it removes dead skin cells and more harmful micro-organisms. It is normal to have a mild odor in the vaginal area. If you notice any changes in the vaginal discharge you should tell your provider.
What Are the Symptoms of Vaginitis?
The symptoms may vary depending on the cause of the vaginitis. Symptoms may include increased or abnormal discharge, pain, dryness, itching, burning, pain with intercourse or with urination. Symptoms may be in the vagina or extend to the vulva.
How Is Vaginitis Diagnosed?
Since there are so many causes of vaginitis, seeing a healthcare provider at the onset of symptoms is crucial. Finding the correct cause and diagnosis of vaginitis begins with seeing a provider and giving a history of your symptoms and medical problems, followed by a vaginal examination. Often the exam may include testing the pH of the vaginal discharge or looking at it under the microscope (wet mount). Sometimes a culture (fungal or bacterial) may be sent which will take a few days. Rarely, a small biopsy of the skin may be required.
How Is Vaginitis Treated?
The treatment of vaginitis depends on the cause of the vaginitis. Treatment may include medications to take by mouth or to place in the vagina. Most of these require prescription by a medical professional. Lubricants or moisturizers may be recommended that can be purchased without prescription. You may also be asked to start a different skin care routine to help keep this skin inside and outside of the vagina healthy.
Causes of Vaginitis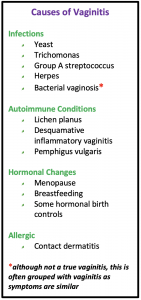
Vaginitis may be related to an infection, autoimmune disease, hormonal condition, or allergic condition. Other causes of vaginal inflammation include irritation (not allergy) to products (soaps, douches, lubricants) used in the vagina, trauma, sexual intercourse without proper lubrication (with a partner, masturbation, or sex toys), or foreign objects in the vagina (tampons, toilet paper, or condoms, for example).
Yeast Infections
This is a type of vaginal infection from a fungus called yeast. Often, a small amount of yeast lives in the vagina without causing symptoms. When large of amounts grow in the vagina, symptoms from inflammation develop.
- Symptoms
Most commonly women have itching and/or burning. This can feel like it is inside or just outside of the vaginal opening. Often these symptoms are accompanied with a thick, white (“cottage cheese”) discharge. Sometimes this discharge is not noticeable to the patient but seen during a medical exam. There is no bad odor.
- Diagnosis
If you have symptoms (itching, burning and/or discharge), a medical professional will do a vaginal exam to collect a sample of discharge (wet mount). If a medical professional looks at the discharge under the microscope, often the yeast can be seen. There is also a change in the pH (acid-base balance) which can be tested during the office visit. Sometimes the yeast cannot be seen under the microscope. In that case, your provider may decide to send a sample of the discharge for a fungal culture.
- Treatment
Antifungal medication can be taken by mouth or placed in the vagina. The most common antifungal medication is fluconazole. Vaginal medication may be preferred if you are pregnant or cannot take oral medications. Treatment of your sexual partner is not necessary.
It is important that you see a medical professional if you think you have a yeast infection. Many times, the same symptoms may be caused by something else. The only way to have the right diagnosis and treatment is to see a medical professional. There are over-the-counter medications which are safe and effective. These medicines will not treat your symptoms if they are from something other than yeast. Trying these medicines before seeking medical care may delay the right treatment for you.
Some women have difficulty with yeast infections that do not seem to go away or they get multiple yeast infections in a year. In these cases, it is important to seek the care of a medical provider each time you have symptoms to rule out other causes of symptoms or the possible need for longer treatments.
- Risk factors
A common risk factor is the recent use of certain antibiotics that can affect the normal bacteria in the vagina. Pregnancy may increase the risk of yeast infection because it causes hormonal changes in the vagina. Diabetes mellitus is another risk factor because it affects a woman’s immune system which is needed to fight infections. Other causes of a decreased immune system, such as HIV (human immunodeficiency virus), can promote yeast infection.
Bacterial Vaginosis
Bacterial vaginosis (“BV”) is not a true vaginitis as it does not cause inflammation. It is often lumped with other types of vaginitis as it causes similar symptoms of increased, fishy-smelling discharge. In women whom have bothersome symptoms and bacterial vaginosis is found, it should be treated to get rid of these symptoms. In women with bacterial vaginosis, there is an imbalance of “bad” and “good” bacteria that normally live in the vagina. “Good” bacteria, called lactobacilli, help maintain a normal pH in the vagina and are usually found in high numbers. For unknown reasons, sometimes there is a shift in bacteria where there are fewer lactobacilli in the vagina and an overgrowth of other types of bacteria. It is not sexually transmitted.
- Symptoms
Vaginal discharge, itchiness, and/or fishy vaginal odor. This does not cause pain and there should be no signs of inflammation on the exam.
- Diagnosis
If you have bothersome symptoms, your health care provider will do a vaginal exam and may take a sample of your vaginal discharge. BV is diagnosed if there is a change in the pH of the vagina and if bacterial overgrowth can be seen when the discharge is looked at with a microscope. The caregiver may also do a vaginal culture test.
- Treatment
Sometimes BV will go away without medical treatment. Many times, oral or vaginal antibiotics are needed to rid the symptoms. These include metronidazole given by mouth or clindamycin, often used vaginally. Both medications require prescriptions from your provider. Your sexual partner does not need to be treated. Metronidazole may cause stomach upset such as nausea or vomiting in some patients. You should not drink alcohol while taking the medication as it can cause nausea and vomiting. Unfortunately, many women may get BV again and require another treatment.
- Risk Factors
Things that may alter the bacterial environment of the vagina increase your chances of getting BV. These include a new sex partner or multiple sex partners or douching. However, BV can also affect women that do not have sex or have never had sex.
Trichomoniasis
Trichomoniasis (“trich,” pronounced “trick”) is an infection of the vagina caused by the micro-organism Trichomonas vaginalis. It is a sexually transmitted infection. It can be passed from a penis to a vagina, a vagina to a penis, or a vagina to a vagina.
- Symptoms
While it is the most common sexually-transmitted disease in the United States, only about a third of those infected have symptoms. Women who have symptoms usually experience itching, burning, soreness, burning with urination, pain with intercourse, and/or a change in vaginal discharge (increase, change in color, fishy odor). Even if you or your partner do not have symptoms you can still pass the infection to another partner.
- Diagnosis
Like the other causes of vaginitis, a medical professional cannot diagnose trichomonas based on symptoms alone. It requires a vaginal examination and viewing the vaginal discharge under the microscope. Your provider may send the vaginal discharge for a lab test which may take a few days. Occasionally, women are diagnosed during time periods when they do not have symptoms but are being screened for other things such as a Pap smear for cervical cancer or vaginal swabs for sexually transmitted infections. Trichomonas can infect the urethra in men and women. The urethra is the opening where urine exits the body. Sometimes trichomonas is diagnosed by urine cultures.
- Treatment
Antibiotics taken by mouth is the main treatment. Metronidazole is the most common antibiotic. It is not safe to drink alcohol with the medication as it can cause nausea and vomiting.
It is important that your sexual partner also be tested and treated for trichomonas. You should wait at least one week after you and your partner have been treated before having sex again. Since about 1 in 5 people may get trichomonas again within a few months of treatment it is important to get tested again if your symptoms return.
- Risk factors
Unprotected intercourse or intercourse with multiple partners can increase your risk of getting trichomonas since it is sexually transmitted. Having yourself and your partner tested for trichomonas and other sexually transmitted infections prior to having intercourse is the best way to prevent the infection. If you have male sexual partners, having your partner wear a condom will lower your chance of getting trichomonas. Sometimes you may still get infected from areas that are not covered by a condom, such as the urethra. You cannot get trichomonas from toilet seats, clothing, or swimming pools.
Atrophic Vaginitis
This condition is caused by decreased levels of estrogen (a hormone made by the ovaries) in the body. This causes the lining of the vagina to become thin, dry, and less elastic. Most commonly this happens after menopause. Menopause is when women stop having their menstrual cycles. Women who develop symptoms from lack of estrogen to the vagina may notice dryness symptoms. These symptoms after menopause are called the Genitourinary Syndrome of Menopause.
Women may develop atrophic vaginitis due to other causes of decreased estrogen in the body. Breastfeeding and some birth control medications, such as Depo-Provera (birth control shot) may also decrease estrogen levels enough to cause vaginitis symptoms.
- Symptoms
Symptoms from lack of estrogen to the vagina may include dryness, irritation, an increase or decrease in vaginal discharge, burning, and pain or dryness with intercourse. Urinary symptoms such as burning with urination and increased risk of urinary tract infections may also occur. Nearly half of menopausal women will experience at least one of these symptoms.
- Diagnosis
To diagnose Atrophic Vaginitis, a health care professional may do a vaginal exam, test the pH of your vagina, or examine your vaginal discharge under a microscope. Women who have gone through menopause and who have symptoms may not need an exam.
- Treatment
The best treatment after menopause is the use of vaginal estrogen. This medication requires a prescription. It is prescribed in several forms: vaginal tablets, vaginal creams, or vaginal slow-release ring insert. Using lubricants (such as KY jelly or similar product) or moisturizers (such as Replens) may be helpful in women who choose to avoid estrogen or for whom using estrogen may be unsafe. The lubricants also can help make sex more comfortable. Newer non-estrogen medications such as selective estrogen receptor modulators (ospemifeme) or DHEA (praseterone) may be treatment options for some patients.
- Risk factors
Menopause is a normal part of a woman’s reproductive cycle. The average age of menopause in the United States is 51 years. Rare conditions may cause early menopause. Women with menopause symptoms for unknown causes at young ages should have a medical evaluation. Some medications such as chemotherapies for cancer treatments may cause temporary or permanent menopause. Breastfeeding and some hormonal birth control methods may cause a temporary decrease estrogen effect in the body causing vaginal symptoms.
Take Home Points
- There are many causes of vaginitis (some are true infections, and others are not) and vaginitis can occur for different reasons throughout a woman’s reproductive life.
- It is important to see your healthcare provider as soon as possible when symptoms arise to ensure proper diagnosis and treatment.
- Call your provider if your symptoms do not go away after treatment.
- Protecting against sexually transmitted infections can help prevent some types of vaginitis.
- Adopting a good hygiene regimen can help prevent vaginitis.
- Estrogen in the vagina can help treat vaginitis in women after menopause.
Author Information
Sarah Bradley, MD is a Female Pelvic Medicine & Reconstructive Surgery physician at Western Carolina Women’s Specialty Center in Asheville, NC. She completed a fellowship at MedStar/Georgetown University in Washington, DC and her residency in Obstetrics and Gynecology at the Mountain Area Health Education Center in Asheville, NC. After residency she spent a year training with Dr. Kiran Sigmon, a specialist in vulvovaginal diseases. Her vulvar clinic receives referrals from all of Western North Carolina. She is a member of the International Society for the Study of Vulvovaginal Disease.
No conflicts of interest to report. The drawings included in the pamphlet are original drawings.