Dee Das, MD
Vulvodynia_FFHA2019
What is vulvodynia?
Vulvodynia is vulvar discomfort or pain lasting for at least 3 months. Pain can be either localized (involving one specific part of the vulva) or generalized (involving the whole vulva). Pain can be provoked (triggered by touch) or spontaneous. The frequency of the pain can also vary, from constant pain to intermittent pain. Most people with vulvodynia have burning pain.
 Pain most commonly occurs with sexual intercourse. Pain can also be triggered by other daily activities, such as sitting or physical exercise. Wearing tight clothing, such as underwear, leggings, or pants, can be uncomfortable. Pelvic exam and tampon use can be painful as well.
Pain most commonly occurs with sexual intercourse. Pain can also be triggered by other daily activities, such as sitting or physical exercise. Wearing tight clothing, such as underwear, leggings, or pants, can be uncomfortable. Pelvic exam and tampon use can be painful as well.
Vulvar pain interferes with the ability to participate in everyday activities. It also affects people’s quality of life and sexual function. It is important to talk to your health care provider if you have symptoms because of the large impact they can have on everyday life and well-being.
Anatomy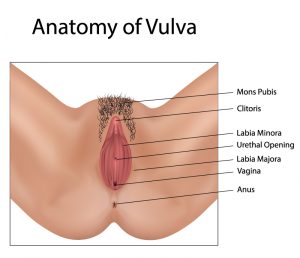
The vulva is external to the vagina. It covers the opening of the vagina. It includes the following organs:
- Mons pubis
- Clitoris
- Labia majora
- Labia minora
- Vulvar vestibule
- Urethral meatus
- Hymen
The clitoris is an organ responsible for sexual excitement. The labia majora and minora (outer and inner lips) are folds of tissue around the opening of the vagina (also known as the vaginal introitus). The urethral meatus is the opening to the urethra, which is a tube that carries urine from the bladder. The area immediately around the urethra and vaginal opening is called the vulvar vestibule.
 Diagnosis
Diagnosis
The exact cause of vulvodynia is unknown. Before vulvodynia can be diagnosed, your health care provider will look for other causes of pain, such as infection, nerve pain, cancer, and trauma. If these are not present, then your provider may diagnose vulvodynia.
Understanding people’s experiences with pain and sexual activity are very important for identifying vulvodynia. The health care provider will ask about:
- pain history
- sexual history,
- previous medical and surgical history.
Your health care provider will then do a pelvic examination. During this, he or she may use a cotton swab to apply light pressure to various areas on the vulva while asking you to rate the pain at each site. Sometimes, a numbing solution is applied to the vulva and the cotton swab exam is repeated.
A speculum exam is often done to assess the vagina. A manual exam is also useful to identify painful areas. During a manual exam the health care provider inserts one finger into the vagina and gently presses on the pelvic floor muscles. During the exam, the provider will collect vaginal swabs to rule out infection. Suspicious areas may be examined with a microscope (called a colposcope) or biopsied. Since vulvar pain can also be related to other parts of the body, the back and hips may be examined.
Treatment
Vulvodynia treatment is focused on reducing pain and improving quality of life and sexual function. Treatment varies by individual and may include the following:
- Vulvar care measures
- Topical medications
- Oral medications
- Physical therapy
- Lifestyle changes
- Cognitive behavioral therapy and/or
- Surgery
Vulvar care
Vulvar irritation can be caused by:
- Creams
- Soaps
- Fragrances
- Deodorants
- Douches
- synthetic lubricants
- tampons
- pads
- vaginal wipes
Avoiding these products can help improve symptoms. The vulvar area should be cleaned gently with water and should be patted dry after. You should not use a hair dryer for drying. An emollient (such as petroleum jelly or vegetable oil) can be applied after gentle cleaning to help hold moisture. You should wear loose fitting cotton underwear. During the night, not wearing any underwear may be helpful. Switching to cotton rather than synthetic menstrual pads can also minimize irritation. For sexual intercourse, adequate lubrication should be used.
Other comfort measures include:
- cool compresses for 10 to 15 minutes
- cool gel packs applied to the vulvar area
- soaking in an Epsom salt bath
- soaking in an oatmeal bath
Topical medications
Lidocaine cream or ointment can be applied before sexual intercourse to reduce pain with intercourse. Estrogen cream may help with vaginal dryness and irritation. Providers may also prescribe specialty creams. All topical medications should be applied only to area that is painful. They are usually applied daily.
Oral medications
Multiple oral medications can be used to decrease nerve pain. These medications are typically started at a low dose and then increased as needed over several weeks. It is important to not start or stop these medications abruptly as this may lead to side effects.
Physical Therapy and Biofeedback
Pelvic floor physical therapy involves exercises to relax and strengthen the muscles of the pelvis. A physical therapist helps perform both internal vaginal and external exercises to help relieve pain and muscle spasms. During physical therapy, a vaginal dilator may be used to help with pain with intercourse.
In biofeedback therapy, counseling is used to teach people how to address pain, manage stress, and regulate pain. Therapy involves multiple sessions over several weeks to months.
Surgery
For women with vulvar pain at one specific area who do not respond to treatments like medications and therapy, surgery is an option. Vestibulectomy is the most commonly performed procedure. This procedure involves removing the painful tissue at the vulvar vestibule. Vaginal tissue is then used to repair the defect at the vulvar vestibule. Surgery has been shown to be very effective at improving everyday vulvar pain and pain with intercourse.
Other
Injections of medications at the site of pain can be helpful. Lifestyle modifications including eating a diet low in oxalate may help decrease inflammation.
Even after improvement with vulvar pain, many people continue to have issues with sexual function. Problems with sexual function may need additional counseling and treatment over time as they can have a significant effect on sexual satisfaction and relationships. Sexual therapy and counseling can be very helpful in improving sexual functioning and satisfaction. This counseling can be done in a group setting, one on one, or as a couple.
Take Home Points
- Vulvodynia is unexplained chronic vulvar pain. This pain affects areas external to the vagina.
- Vulvar pain can affect daily activities.
- Vulvar pain can cause pain with sexual intercourse and affect people’s ability to participate in and enjoy sexual intercourse.
- There are a variety of treatments, including behavioral, medical and surgical treatments, that can help improve vulvodynia symptoms. Your gynecologist can provide more information about each of these treatment options.
- Problems with sexual function can continue even after vulvar pain improves. Sexual counseling and therapy can help address such problems.
Additional Resources
- National Vulvodynia Association: https://www.nva.org/
- American College of Obstetricians and Gynecologists: https://www.acog.org/~/media/For%20Patients/faq127.pdf
References
- Stenson AL. Vulvodynia: Diagnosis and Management. Obstet Gynecol Clin North Am. 2017;44(3):493-508. doi:10.1016/j.ogc.2017.05.008
- Haefner HK, Collins ME, Davis GD, Edwards L, Foster DC, Hartmann EH et al. The vulvodynia guideline. J Low Genit Tract Dis. 2005;9(1):40-51. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed10&NEWS=N&AN=40116727.
- Persistent Vulvar Pain: Committee on Gynecologic Practice. ACOG Committee Opinion: Clinical Management Guidelines for Obstetrician-Gynecologists, Number 673.; 2016.
Author Information

Dee Das, MD is a resident physician in Obstetrics and Gynecology at the Cleveland Clinic. She completed her undergraduate medical education at the University of Virginia. She has no conflicts of interest to report.