Pelvic organ prolapse or vaginal prolapse is a condition where your uterus (or “womb”) or vaginal walls sag down and create the feeling of a bulge in your vaginal area. This condition is very common. If you have prolapse, you also may develop problems moving your bowels or urinating.
What are the symptoms of prolapse?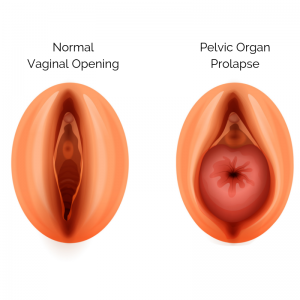
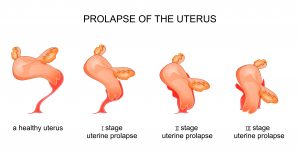
One of the most common symptoms of prolapse is a bulge in the vaginal area. Some women only have this symptom, but some may have symptoms such as difficulty moving their bowels or emptying their bladder. The kind of symptoms you have depends on which of your pelvic organs are causing the bulge. Apical prolapse occurs when your uterus sags downward (“uterine prolapse”) or when the top of your vagina bulges downward after you’ve had a hysterectomy. Anterior prolapse happens when the vaginal wall next to the bladder sags. This type of prolapse, also called a “cystocele”, can be linked to bladder problems. Posterior prolapse is when the vaginal wall sags in the area next to the part of the bowel where your stool passes right before it leaves your body (rectum). This type of prolapse, also called a “rectocele”, can cause difficulties passing stool easily. If you have prolapse symptoms, you may have one, two or all three of these types of prolapse. Your medical provider will need to do a vaginal exam to tell which kind of prolapse you have.
Who can get prolapse?
Prolapse is more likely to affect women who have delivered babies, and it gets more common with age. Many women who have prolapse are embarrassed to speak about their problems, so you might have friends, colleagues, or family members who have this condition without knowing they suffer from prolapse or seeking treatment for it.
Why do women develop prolapse?
There are a number of reasons why women develop prolapse. If you have a relative who has prolapse, then you are more likely to develop prolapse. Pregnancy and vaginal delivery can damage structures in the pelvis that support your vagina and pelvic organs and can also lead to prolapse. The decrease in the hormone estrogen that happens when women stop having periods at menopause can also contribute to worsening of prolapse symptoms. Having medical problems such as obesity, chronic cough, or constipation can put a lot of stress on your pelvic floor and put you at higher risk for prolapse.
Is prolapse dangerous? What kind of problems can I develop if I have prolapse?
Prolapse is not dangerous. It is not a tumor. Some women fear that their uterus or vagina will fall out of their bodies. While you might feel a bulge, your uterus and vagina will never completely fall out of your body. Your vaginal bulge may be uncomfortable. If the bulge rubs against your underwear, then you can see vaginal spotting or bleeding. You may also be bothered by not being able to move your bowels normally and control your bladder, but these symptoms, though bothersome, are not dangerous to your health. You also may have sexual problems such as pain with sex or difficulty having sex.
If I have prolapse or think I might have prolapse, when should I go see a medical provider?
If you think you have prolapse and are bothered by any symptoms related to prolapse, then you should go see a medical provider. Not all medical providers know about prolapse or how to treat prolapse, so be sure to find a provider who specializes in prolapse or ask your provider to refer you to a specialist. Physicians who have special training in prolapse and incontinence are called urogynecologists or female urologists.
 What treatments are there for prolapse?
What treatments are there for prolapse?
There are a number of options for the treatment of prolapse. Your medical provider might recommend one of these options or a combination of these options.
- Nothing
- Since prolapse is not dangerous, if you are not bothered by your symptoms, then you can choose to do nothing. If your prolapse symptoms get worse, then you can return to your medical provider, and let them know when you are ready to try something to treat your symptoms.
- “Kegel’s exercises” or Pelvic floor physical therapy
- Pelvic floor physical therapy (PFPT) is a type of physical therapy that focuses on the muscles that support pelvic organs, such as your bladder, vagina and uterus. PFPT can help with bulge symptoms or urinary incontinence by strengthening the pelvic floor muscles. You will have to see a physical therapist who specializes in the pelvic muscles. You may have to go to therapy as often as once a week for up to 6 weeks. Your physical therapist may teach you how to do exercises at home. Kegel’s exercises are one of the ways to strengthen the pelvic floor muscles. Your physical therapist, gynecologist, or midwife will make sure you are performing these exercises correctly. This is a very low-risk approach to managing prolapse and its symptoms. Your medical provider may recommend that you do physical therapy in addition to other treatments.
- Pessary
- A pessary is small, flexible plastic device that you place in your vagina that holds the vaginal bulge in place so that you can no longer feel the bulge. Your provider might show you how to put in and replace the pessary yourself. If you don’t want to or can’t place the device in your vagina or remove it by yourself, then your medical provider can do it for you. The pessary can be cleaned easily with soap and water. You can leave the pessary in your vagina for up to 3 months at a time without changing. You are not supposed to be able to feel the pessary when it is in your vagina. When the pessary is removed, your prolapse will return. It is a low risk option to treat prolapse without surgery, but it requires regular attention.
- Surgery
- Some women want a more permanent option to treat their prolapse. Your medical provider may recommend surgery if you do not want or cannot use a pessary, if you have tried physical therapy without relief of your symptoms, and if you are healthy enough to undergo surgery. There are many different kinds of surgery for prolapse. The kind of surgery that your doctor recommends depends on what kind of prolapse you have, your past medical and surgical history, your lifestyle, and your goals for surgery. You may have surgery through the vagina using structures in your body to help support the prolapsed vaginal walls or uterus. Or you may have surgery through small incisions in your abdomen. You may have a permanent material called mesh added to your surgery to help support your tissues if your doctor believes it is necessary. Please speak with your doctor about the risks and benefits of each surgery. Make sure your goals align with the surgery they plan.
Take Home Points
- Prolapse is a common condition that affects many women. Women with prolapse can have a sensation of a bulge, difficulty moving their bowels or emptying their bladder, or have problems having sex.
- Many factors can cause prolapse. Prolapse is not dangerous, but make sure you see a medical provider if your symptoms bother you.
- There are many ways to treat prolapse. Talk to your medical provider about all the options, and decide which one is the right one for you.
Additional Resources
https://www.thewomens.org.au/health-information/vulva-vagina/vaginal-prolapse
https://vcgmedia.objects.frb.io/ucurogyn/Pelvic-Organ-Prolapse__IUGA_UroGyn.pdf
https://www.augs.org/assets/2/6/POP.pdf
Author Information

Emi Bretschneider, MD
Assistant Professor, Department of OB-GYN,
Urogynecology & Reconstructive Pelvic Surgery,
Northwestern Medicine, Chicago, IL, USA
No conflicts of interest to report.